Otorhinolaryngology
Pneumology
For all your repairs
Asthma always
more frequent ?
by Elisabetta Bocci
05/29/2024






Asthma
Origins, symptoms, treatment and management
Introduction
Asthma is a chronic respiratory disease that affects millions of people worldwide. Its prevalence is increasing, probably due to various environmental and socio-economic factors. As a general practitioner, it is crucial to understand the different aspects of this disease in order to offer patients optimal care.
Origins and causes
-
Genetic factors: Heredity plays a significant role in the development of asthma. A family history of asthma or other atopic diseases (such as eczema and allergic rhinitis) increases the risk of developing the disease.
-
Environmental factors :
-
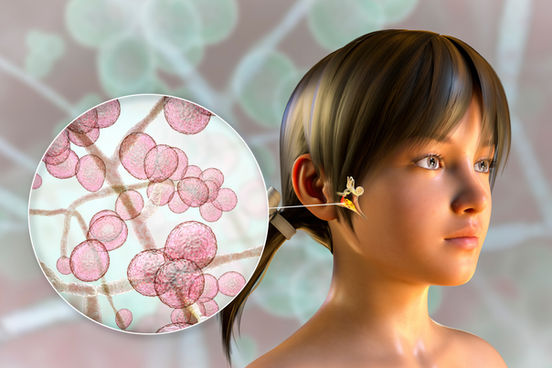
Allergens: Household allergens such as dust mites, mould, pollen and pet dander are common triggers.
-
Air Pollutants: Exposure to high levels of air pollution, tobacco smoke and industrial chemicals can exacerbate asthma symptoms.
-
Respiratory infections: Viral infections in childhood, particularly those caused by the respiratory syncytial virus (RSV), are associated with an increased risk of asthma.
-
-
Hygienist hypothesis: This theory proposes that the reduction in exposure to infectious agents in industrialised countries has led to an increase in atopic diseases, including asthma.
Clinical manifestations
Asthma symptoms can vary in frequency and severity:
-
Cough: Often nocturnal or morning cough.
-
Wheezing : Presence of sibilance on exhalation.
-
Dyspnoea: Feeling of shortness of breath.
-
Thoracic tightness: Sensation of constriction in the chest.
Diagnostic
The diagnosis of asthma is based on a combination of clinical and paraclinical factors:
-
History: Look for a family history of atopy, symptoms triggered by allergens or physical exertion, and seasonal variations.
-
Physical examination: Identify clinical signs such as sibilance and thoracic hyperinflation.
-
Respiratory Function Tests (RFT) :
-
Spirometry: Measurement of FEV1 and FEV1/FVC ratio before and after bronchodilator treatment.
-
Reversibility test: improvement in FEV1 of more than 12% and 200 ml after inhalation of bronchodilator.
-
Peak Flow: Measurement of peak expiratory flow to assess symptom variability.
-
Treatments
-
Basic treatment :
-
Inhaled corticosteroids (ICS): First-line treatment to reduce bronchial inflammation.
-
Long-acting beta-2 agonists (LABA): Used in combination with ICS to improve symptom control.
-
Leukotriene receptor antagonists: alternative or complementary to ICS.
-
-
Emergency treatment :
-
Short-acting beta-2 agonists (SABA): Used for rapid relief of acute symptoms.
-
Inhaled anticholinergics: Used in the event of a severe attack or as a complement to SABA.
-
-
Biological therapies :
-
Indicated for severe asthma refractory to conventional treatments (e.g. anti-IgE, anti-IL-5).
-
Management and prevention
-
Patient education: the importance of recognising and avoiding triggers, correct use of inhalers and adherence to treatment.
-
Personal Action Plan: Develop a written plan for managing asthma attacks, including the steps to follow in the event of an exacerbation.
-
Vaccinations: Influenza and pneumococcal vaccinations are recommended to reduce the risk of respiratory infections.
-
Regular follow-up: Monitoring the progress of the disease, adjusting treatments and checking inhalation technique during follow-up consultations.
Conclusion
Asthma is a complex disease requiring a multidisciplinary approach for effective management. As a GP, it is crucial to keep abreast of the latest advances in asthma treatment and management to improve patients' quality of life. Personalised management, based on comprehensive assessment and regular monitoring, is essential to control this chronic disease and prevent exacerbations.
Lagap SA offers an interesting range of anti-asthma products, one of which is specially formulated for children, even infants.